One baby, one heart, one huge leap
Dr. Lori West will never forget that moment. It was on a wintry night in 1996. She took her place alongside the surgical team filing into an operating room at SickKids Hospital in Toronto, with a very sick baby named Caleb, who was just weeks old.
Caleb was born with hypoplastic left heart syndrome, one of the deadliest heart defects, and was expected to live for just a few weeks. His only hope for survival: a new heart. Amazingly, an infant donor heart had become available. But Caleb’s blood type did not match that of the donor. In organ transplants, this was the number one rule: the recipient’s blood type — whether A, B or O — must be a match. If not, the donor organ will turn black and essentially die on the operating table once blood starts flowing through it.
Dr. West, a pediatric cardiologist with a PhD in transplant immunology, had been researching infant heart transplants. She knew that babies have immature immune systems that do not yet generate antibodies against other blood types.
So, she asked what no one else had ever dared: Could a baby accept an organ from a donor with a different blood type?
Dr. West reviewed the literature, ran preliminary tests and had extensive discussions with the surgical transplant team and medical ethics panel. She was confident her theory would prove correct. Next, she shared her findings with Caleb’s parents and earned their trust. They consented to let their child be the first to receive a donor heart with an incompatible blood type.
Now the moment had arrived. As she walked into the operating room that night, Dr. West felt a hand on her shoulder. The lead surgeon leaned over and said, “You better be right about this.”
The drama of that moment encapsulated years of fighting for children and families with no hope. A Heart & Stroke-funded researcher both then and now, Dr. West told us the story of this dramatic first.
What first got you interested in transplant medicine?
I realized that being a pediatric cardiologist was not sufficient. You needed to have a sub-specialty. With organ transplants, there were some opportunities that were becoming very exciting.
When I came to SickKids for a fellowship, no one was focused on moving pediatric heart transplantation forward. It appealed to me because these were life-and-death decisions.
So, I went to Oxford University to study the basic science of transplant immunology. I was the only cardiologist in the group, the only one who had an interest in heart transplants, much less pediatrics. I came back to SickKids four years later with a PhD and a baby. That’s when I took on the role of medical director of the heart transplant program.
What is hypoplastic left heart syndrome?
It’s one of a group of heart defects we call single-ventricle malformations. Hypoplastic left heart syndrome, where the heart’s left side is underdeveloped, is probably the most common of these. Previously it was often referred to as ‘the worst heart disease,’ because there was no cure for it.
What did you tell parents of babies born with this syndrome?
In the early 1990s, we would counsel parents about three options. The first was to do nothing, and their baby would pass away – these are lethal malformations.
The second option was a series of heart surgeries over a few years. The kids are very, very sick going into this surgical pathway, but you may be able to buy them some time. Even then, the results were pretty grim back then.
The third option was a heart transplant. We’d say, “We’ll list your baby for a transplant, but you have to understand it’s very unlikely that we’ll get a donor organ.”
So, there were no good options for these babies. How did that make you feel?
I was very junior in those days. But my field, to me, seemed to have a collective shrug about hypoplastic left heart syndrome.
After all, it's the worst heart disease. The attitude was kind of like, “Go home and try again.”
I found it very troubling that we couldn't do more for these children.
What did you do to change that?
I began to think about how to expand the donor pool for infant heart transplants.
First, I wrote about 300 letters to every organ procurement organization in the United States, just to say, “We're in Canada. We're here! If you have organs you can't place, please send any referrals our way.”
Then one day I had to turn down a donor offer because it was the wrong blood group. The baby died. That’s when it just smacked me right in the face: Most of these kids are never going to get transplanted and we were declining donor offers.
So, I began to think about asking: Why are we saying it’s absolutely necessary to have blood group compatibility?
What obstacles did you face in exploring this idea?
This was like a sacrosanct barrier. You wouldn’t even let your mind go there, that you could cross the ABO (blood group) barrier, because the consequences would be so catastrophic.
And I was a very junior cardiologist to be proposing such a huge step forward.
To cross the blood group barrier in kidney transplantation is one thing, because the patient can go back on dialysis if it doesn't work. With heart transplantation, if it doesn’t work, your patient is going to die.
But as I learned more about it, I realized that the rules that we live by in transplantation were based on certain assumptions. One was that we didn’t generally transplant infants.
What was your perspective on infants as transplant patients?
I had done a lot of research on the immature immune system. It was well known that babies don't make ABO antibodies. Also, because the waiting-list mortality was so high for these infants, you had a compelling patient population. So, I began to think about it scientifically and talk to people in hematology and other relevant areas.
Fortunately, we had quite a forward-thinking surgical team at SickKids, and they were interested in pushing the traditional boundaries.
I took a lot of time to really understand the science in depth; it was in the scientific literature that I found most of the information I needed. And that helped me build a rationale as to why this was an entirely reasonable pathway to suggest.
How did you find a family willing to take this risk with you?
I remember the first phone call. It was to a family in Winnipeg. Their baby was not yet born, but he had a fetal diagnosis of hypoplastic left heart syndrome.
I talked to them for a couple of hours that day. I outlined those three options that we gave families at that time. And I talked about the potential for a transplant with an incompatible blood group.
They were interested in hearing more. They came to Toronto when the mother was 36 weeks pregnant. After their baby was born, he was listed for a donor heart. They waited, and he got more fragile as three weeks went by.
And then there was a call one night.
Take us through those hours leading up to the surgery.
There was a donor heart offer for Caleb, but it was not his blood group.
His parents knew this type of transplant had never been done. But they understood the risks and were receptive to new approaches that came from research.
When the offer of an organ came through, they didn’t have much time to decide. They thought about it for a little while, then came back and said they thought this was the best opportunity for their child. And so, we went ahead.
How did you feel when the surgeon said, “You better be right about this”?
Oh my gosh. It sort of felt like a kick in the gut. I thought, “What if I'm wrong? What if I'm wrong?”
I went back out into the corridor, and I called a colleague who had a very calm manner. He said, “You've thought this through. It’s going to be fine; don’t worry.” That assurance helped.
Then the operation proceeded. At that point it became almost routine. You’ve made your decision; you’ve got to get through it. But still, as I leaned over the table watching, there was sweat trickling profusely down my back.
When did you know if the operation was successful?
The surgical team took off the clamps to let blood flow into the heart. The heart didn't start instantly. Sometimes for a few seconds, you don't know. But you wait a little bit, or sometimes you go back on pump. I think we just waited.
Then the heart started, and then it was fine.
When we came back to the intensive care unit from the operating room that morning, Caleb’s father noticed that it was February 14. “What a wonderful Valentine’s Day!” he said.
That was 1996. How did this transplant change practice?
The ability to transplant infant hearts from incompatible donors meant that the donor pool for any given infant candidate increased significantly. Plus, over the next two years we saw a decrease in the number of babies dying on the wait list from more than 50% to less than 10%.
Now this practice is routine at pediatric transplant centres worldwide.
And it continues. Just this morning, I got a message from a colleague at the University of Florida saying, “We've just done this transplant, there’s this thing… can you tell us about this thing?” There was a similar call from Newcastle in England last week.
What role did Heart & Stroke research funding play in this breakthrough?
I can't remember the year I had my first Heart & Stroke grant; it may have been 1994, not long after I was appointed to faculty at SickKids. That started me down this pathway, because then we could do the experiments to generate the preliminary data for the publications.
This in turn would allow us to get a renewal grant, because we had made progress. So, for my own research, Heart & Stroke support has been invaluable. I don’t think I could have gone anywhere without those first grants.
You’re still receiving Heart & Stroke funding. What are you researching now?
My lab now works almost full-time on research related to the ABO blood groups, specifically in transplantation.
One of the advantages of being at the University of Alberta, where I moved in 2005, is that there’s a decades-long history of carbohydrate chemistry expertise here. This has allowed us to move into a different side of research, looking at the basic chemistry that makes up the structures of the ABO system.
We’ve worked with these chemists to create a new blood test that brings much more precision, reliability and accuracy to testing for ABO antibodies. We think this is going to be a big step forward – including for heart transplants beyond infancy.
And there’s still so much work to do on transplantation. It would not be accurate for us to gloss over the problems that people face after an organ transplant. For some, it’s a challenge adhering to the medications they need to take. For others, they may experience side effects from years of immunosuppression, which can mean they may eventually need a kidney transplant.
So, transplantation is not the answer to everything. It’s the answer that starts a patient down their pathway; at least it gives them a chance at life. But we always need to do better, and we can only make advances with continued research.
How does it feel knowing that your research helped save the lives of children around the world?
Research has many impacts, but few that are quite as deeply meaningful, where you can say, this discovery actually had a direct impact on the lives of these families and these children, in the real sense of life and death.
It reminds me of an email I received from Caleb around the time he turned 18. He wrote to me on Valentine's Day, because that’s his transplant anniversary. He said, “I thought this would be a good time to just say thank you for my life.”
- Learn more about congenital heart disease
- See how your donations are saving lives

Real stories, real impact

The gift that keeps on beating
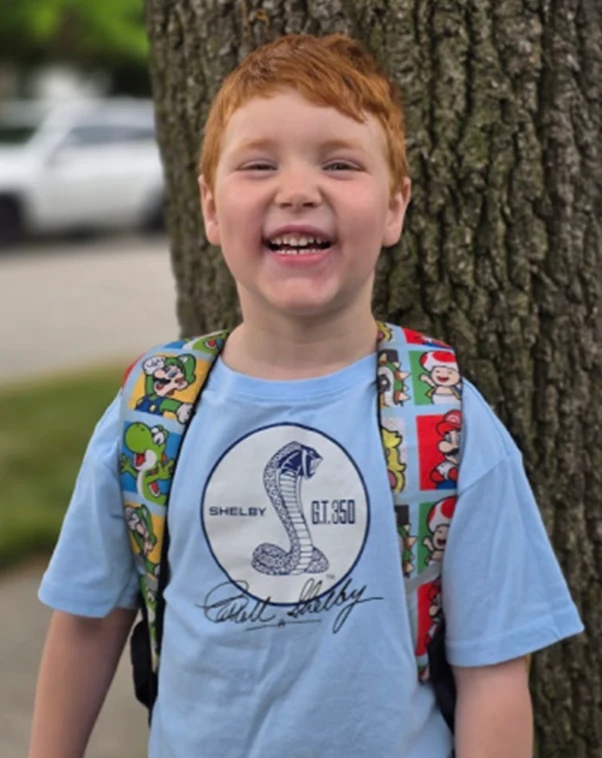
For Logan survival was just the beginning

A spark that shines bright